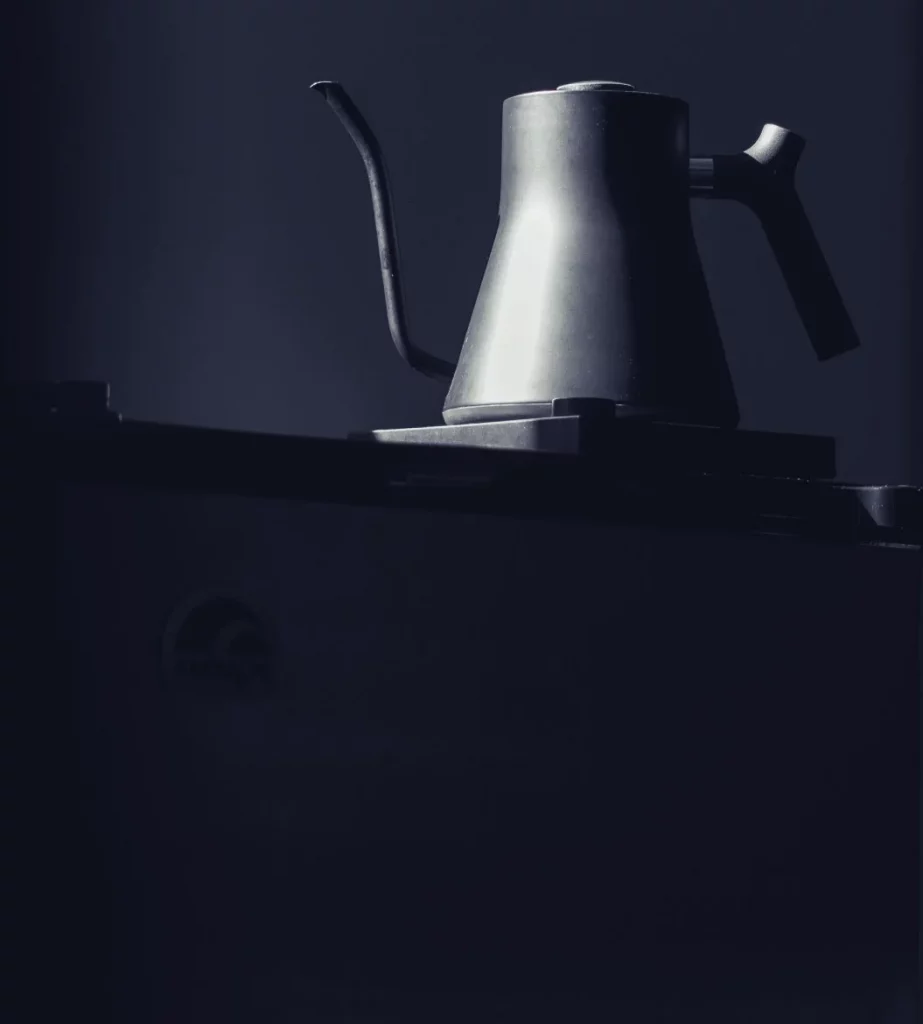
On a cold morning in February, seven stainless steel electric tea kettles, filled with hot water, were delivered to patients’ rooms at UC San Diego Medical Center in Hillcrest. The tea kettles were not typical, but neither were the times. The Covid-19 pandemic had begun in earnest, and the kettles represented an early act of comfort and humanity, in a time that would soon demand an outpouring of both.
The COVID-19 pandemic had begun in earnest, and the kettles represented an early act of comfort and humanity in a time that would soon demand an outpouring of both.
On February 5, 2020, UC San Diego Health activated the organization’s Hospital Command Center (HCC), the central location where in-house experts gather to develop and implement a response to an emergent and urgent situation. In this case, it was the growing crisis surrounding the novel coronavirus, SARS-CoV-2, then rapidly spreading in Wuhan, China.
Five days later, UC San Diego Health received its first patient with diagnosed COVID-19, an evacuee from Wuhan, who had previously been airlifted to and quarantined at Marine Corps Air Station (MCAS). The patient was officially the 13th case of COVID-19 in the United States and would soon be followed by others from MCAS.
They arrived via ambulance, escorted by law enforcement vehicles and greeted by medical staff, security officers and officials from the Centers for Disease Control (CDC), all wearing masks, face shields, gloves and other personal protective equipment (PPE).
Seven new tea kettles were purchased, filled with hot water and served with sides of lemon and ginger to the first patients from Wuhan.
There were more questions than answers

The virus was largely unknown, as was the plan of treatment. There were more questions than answers.
“One question raised in the HCC was ‘Does anyone here speak Mandarin?’” recalled Lily Angelocci, transformational health care lead coach at UC San Diego Health. “From there, I spent the next two weeks at the bedside of the patients in our intensive care unit, helping to meet their physical and emotional needs.”
Four evacuees were eventually transferred from MCAS to UC San Diego Health for care. Most spoke little or no English. Translators were found.
Angelocci was always nearby, intent on addressing their physical needs or easing their emotional concerns. It wasn’t yet clear who was infected with the SARS-CoV-2 virus and who was not, but all of the patients were far away from home, away from loved ones and afraid of a disease no one yet understood.
“At the time, we had to wait days to receive test results from the CDC in Atlanta to confirm if the patients from Wuhan were actually positive with the virus,” said Angelocci. Two were.
“What initially struck me was the delicate humanity of the situation,” said Francesca Torriani, MD, program director of Infection Prevention and Clinical Epidemiology at UC San Diego Health. “In the patients’ faces, I could simultaneously see fear and gratitude: fear of rejection and gratitude for us accepting and welcoming them.
“Can you imagine being evacuated from Wuhan on a windowless airplane, not knowing if you had the virus, or if you would live or die; of being targeted because of bringing a new disease into a country? My heart went out to them.”
Even with the language barrier, the patients’ concerns and fears soon became apparent.

Comfort Food

“We realized that they were not eating,” said Jill Martin, director of food and nutritional services at UC San Diego Health. “We needed to devise a plan to make sure these patients were fed and felt supported. Our role is not just to provide food on a tray. Providing healthy meals is a significant part of the recovery process. That was our main priority.”
Many of the patients could not digest certain foods being offered.
With assistance from Angelocci, Martin’s team visited specialty grocery stores to purchase more familiar fare. It brought patients and staff closer together. “One of our chefs, Bo-Kai Liao, speaks Mandarin and was integral in those early days, making sure there was a strong line of communication. He would call the patients in their rooms several times a day, find out about their food preferences and customize their meals,” said Martin.
Favorites were wonton soup, egg and seaweed soup, congee (a type of rice porridge), spicy Mapo tofu and a Taiwanese basil omelet.
Meals were served using only disposable materials, to reduce the risk of virus transmission. Some foods, such as meats, were cut into bite-sized portions in the kitchen before delivery.
“We are all human, but different things comfort and heal us,” said Martin.
“We found a balance of caring for these patients while still following all the safety measures.”
“Normally, loved ones are in the rooms to help with the meals, but that was not the case for these patients. Sometimes, patients were too weak to cut their own food, so we did that for them to make sure we were doing everything we could to help them eat and heal.”
The seven tea kettles were part of that process.
“In Chinese tradition, they do not drink cold or room temperature water, only hot water. In talking with the patients, we realized they were being served cold water,” said Angelocci.Tea kettles were purchased. Patients soon received their water hot, served with sides of lemon and ginger. Patient Experience staff added to the efforts, delivering floral arrangements to brighten up rooms and power cords, chargers and coloring books to help patients stay connected to the outside world and pass the time.
“We always teach our staff one word: the Japanese term, ‘gemba’,” said Angelocci.
“It means ‘the place where value is created.’ In practical terms,” said Angelocci, “it means to ‘see, show respect, and ask why.’ It meant the world to patients and staff.”
— Jill Martin“We needed to devise a plan to make sure these patients were fed and felt supported. Our role is not just to provide food on a tray. Providing healthy meals is a significant part of the recovery process. That was our main priority.”